Excess Mortality and COVID-19 Deaths: Preliminary Data from Serbia and Comparison with European Experience
Daniela ArsenovićA
Received: October 12, 2022 | Revised: February 11, 2023 | Accepted: February 27, 2023
doi: 10.5937/gp27-4062
A University of Novi Sad, Faculty of Sciences, Department of geography, tourism and hotel management, Trg Dositeja Obradovića 3, 21000 Novi Sad, Serbia; daniela.arsenovic@dgt.uns.ac.rs
Abstract
Mortality statistics is underlay for public health measures and action and consequently it is one of the major indicator in measures of Covid-19 impact on population. This study aim to explore excess mortality during the Covid-19 pandemic in Serbia. Excess mortality compares expected and observed number of deaths during the given period. Analysis in this paper was based on excess deaths and excess mortality rate. Data was downloaded from the national COVID-19 database and obtained from a relevant source from the Statistical Office of the Republic of Serbia. In order to provide better understanding of excess death, the excess mortality rate was calculated for the period January 2015-June 2022. For the period January 2015-February 2020, 38 months were observed without excess deaths, while in months with excess deaths, almost in all months excess mortality rate was below 12%. Since March 2020, the excess mortality rate has increased significantly, with highest values in December 2020 (91.4%), October (84.3) and November (67.8) 2021.
Keywords: excess mortality rate; excess deaths; Covid-19; pandemic; Serbia
Introduction
The first Covid-19 cases in China were reported in December 2019, spreading quickly to neighbouring countries and then across other regions including Europe (Michelozzi et al., 2020). The Covid-19 pandemic has been declared on March 11 2020 by the World Health Organization and continuously world population stands up to new health, economic and societal issues and challenges. Over 560 million confirmed Covid-19 cases, including more than 6 million deaths have been reported globally1. According to the data from Ministry of Health and Institute for Public Health of Serbia „Dr Milan Jovanović Batut“ in Serbia, more than 2 milion persons have been diagnosed with virus and more than 16 thousand deaths were related to the Covid-19 (on July 21 2022). The Covid-19 has brought various concerns regarding the demographic and epidemiological consequences. Therefore, since January 2020, many studies and research papers have been published, addressing of Covid-19 disease, risk and prevention (Arsenović, 2020), as well as demographic, economic and social consequences. According to Hulikova Tesarkova (2020), first studies were oriented on biological, medical, epidemiological and medical issues. In a short time they were followed with demographic approaches. Population age structure was highlighted as one of the main determinants in Covid-19 pandemic (Balbo et al., 2020; Dowd et al., 2020). According to the Dowd et al. (2020) countries with higher proportion of older population are at higher risk under the coronavirus and age structure could explain differences in fatality rate as well as transmission pathways. The role of age structure play important role, but population diversity is important too, since the young population in metropolitan areas, certain ethnic groups, male population and those with chronic diseases, have also been affected by the virus (Balbo et al., 2020). Role and impact of demographic determinants varies across regions. Research conducted in Wuhan (China) shows that small places with weak gravitational forces are more likely to contribute to quickier spreading across the country (Kustudic et al., 2021). Investigation across 23 European countries found that social and economic factors are strongly associated with Covid-19, while the impact of population density and cultural factors was low (Mogi & Spijker, 2021). Findings for Slovakia, analysis of lethality shows that areas with very high lethality but also with very low lethality, are located as isolated regions in country (Michalek, 2022).
The impact of Covid-19 on a population of given country is usually assessed using the two indicators: number of cases and number of deaths (Karlinsky & Kobak, 2021). These two metrics have been reported on daily level by each country and merged into international database such as the ones maintained by World Health Organization or by the Johns Hopkins University (Dong et al., 2020; Karlinsky & Kobak, 2021). Usage of this datasets is limited due to diverse methodological aprroaches in how Covid-19 deaths are reported. The World Health Organization defines a Covid-19 death as one where Covid-19 is the underlying cause of death, including both confirmed and suspected cases (Beaney, 2020). However, in Russia, confirmation of Covid-19 death relies on results from autopsy. In Spain only hospital Covid-19 deaths are included in the death count, while in Belgium, all suspected cases are included in Covid-19 mortality (Beaney et al., 2020; Marinković & Galjak, 2021a). Divergency between countries may also vary with respect to different demographic, medical, economic and social drivers of spreading Covid-19.
Additionally, available mortality data about Covid-19 could be underestimated for several reasons. Absence of testing and low rates of diagnoses at the beginning of pandemic, and less known complication of Covid-19 related to the coagulopathy, myocarditis, inflammatory processes and arrhythmias could lead that some Covid-19 deaths were assigned to other causes (Boukhris et al. 2020; Driggin et al., 2020; Del Pinto et al., 2020; Gill & DeJoseph, 2020; Stokes et al., 2021). Also, Covid-19 deaths do not counts cases linked with indirect impact of pandemic-limited access to the medical services, psychological stress, economical issues etc. (Stokes et al., 2021).
Regarding to the Covid-19 deaths, lockdown and other restrictions have increased deaths from chronic and acute diseases due to limited access to the medical services (Wang et al., 2022) and death from self-harms due to crisis of psychological well-being (Sierra et al., 2020). Recent study (Sher, 2020) confirmed that increases stress and depression related to the pandemic could result with suicides and overdose deaths too. Furthermore, economic circumstances, such as housing and food insecurity, could increase death, particularly among population with some pre-existing chronic conditions (Stokes et al., 2021). Simultaneously, pandemic decrease deaths from specific external causes linked to road accidents (Wang et al., 2022), sports, nightlife and work accidents (Sierra et al. 2020).
As a effective way to quantify the direct and indirect impact of Covid-19 on all-cause mortality, many studies as metric used excess mortality (Arsenović, 2020; Arsenović, 2021; Blangiardo et al., 2020; Wang et al., 2022; Konstantinoudis et al., 2022; Islam et al., 2021; Vandoros 2020). This measure was used for regional estimation, country level and specific location, counting excess death in various stages of pandemic. This paper aims to analyse and to give insights into the number of all-cause excess mortality (January 2015-June 2022) and COVID-19 death (March 2020-June 2022) in Serbia. Since the COVID-19 pandemic is still in progress, data and results presented in this research are preliminary.
Data and methods
In the analysis was used data from the national COVID-19 database2, where data about confirmed cases and reported deaths are available. COVID-19 data was downloaded for the period from 6th March to 30th June 2022. As the available data from the national Covid-19 database provide information daily, the data was aggregated on a monthly level. Research was constrained only to the total number of Covid-19 deaths, due to the lack of data in Covid-19 database (i.e data by gender and age was not available for the observed period).
In order to assess excess mortality total number of deaths by month was obtained from the Statistical Office of the Republic of Serbia (SORS), for the period since 2010, while excess mortality was calculated from January 2015 until June 2022. Mortality data for January 2010 until December 2014 was provided from the following reference: SORS 2015. Data for January 2015 until December 2021 was extracted from SORS online database3, while for the period January-June 2022 data was extracted from SORS Population Statistics Report (RZS, 2022). Data from these two sources (SORS online database and Population Statistics Report) may vary and since 2022 is still in progress, final mortality statistics at the end of the year could count different numbers of deaths. Excess mortality can be measured in different ways. In this paper the excess mortality defined as the observed minus the expected number (average number of death in the baseline period) of deaths in month Mi was estimated as:
ED (Mit+n) = OD (Mit+n) – AND (Mit,t+n)
were:
- ED – Excess deaths
- OD – Observed deaths
- Mit+n – observed month
- AND – Average number of deaths
- Mit,t+n – historical baseline from previous years
The excess mortality rate was calculated as the percentage difference between the number of deaths in Mit+n and the average number of deaths in the same month (Mit,t+n) over the historical baseline period.

were:
- EMR – Excess mortality rate
In this paper, the historical baseline consists of the average number of deaths that occured in each month in the five year period before observed year. Excess mortality for the 2020, 2021 and first half of 2022 was calculated using historical baseline from previous years in a period which was not affected by the Covid-19, considering the number of deaths that occurred in each month during the period 2015-2019.
Results and discussion
Serbia reported the first case of Covid-19 on the 6th March 2020. Nine days later (March 15th), a state of emergency was declared in the country and in order to reduce transmission, the whole population was lockdown. All public sectors were redirected to telecommuting, while other places of services and for public gathering were closed. Regardless of all country-wide measures during March 2020, transmission of Covid-19 was very fast and intense. Fast transmission in this period could be related to the fact that about 300,000 of Serbian residents arrived from abroad (Arsenović, 2020). After two months, on May 7th 2020, the government ended the state of emergency, with recommendation and not very restrictive social distancing. Since second half of June 2020, large-scale testing was conducted and the number of new confirmed cases and number of deaths due to Covid-19 has started to increase (Arsenović, 2020). During the second half of 2020 and the whole 2021 government applied different restrictions regarding the reduced or limited working time in public administration and services (e.g. restaurants, bars and markets), but without lockdown. Since the beginning of 2022 these restrictions have been withdrawn.
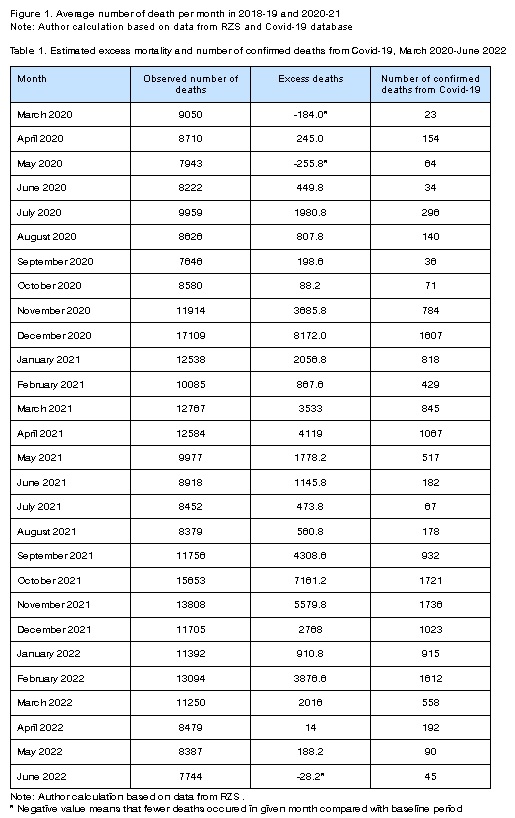
With exception in February, the average number of monthly deaths during the Covid-19 pandemic years 2020-21 was higher in all other months compared to the average number of monthly deaths in two preceding years 2018-19 (Figure 1). Divergence in average number of monthly deaths has ranged from 665 (in August) to 5 665 (in December) when it was recorded the highest number of deaths and excess deaths too.

Figure 1. Average number of death per month in 2018-19 and 2020-21
Note: Author calculation based on data from RZS and Covid-19 database
Table 1. Estimated excess mortality and number of confirmed deaths from Covid-19, March 2020-June 2022
|
Month |
Observed number of deaths |
Excess deaths |
Number of confirmed deaths from Covid-19 |
|
March 2020 |
9050 |
-184.0* |
23 |
|
April 2020 |
8710 |
245.0 |
154 |
|
May 2020 |
7943 |
-255.8* |
64 |
|
June 2020 |
8222 |
449.8 |
34 |
|
July 2020 |
9959 |
1980.8 |
296 |
|
August 2020 |
8626 |
807.8 |
140 |
|
September 2020 |
7646 |
198.6 |
36 |
|
October 2020 |
8580 |
88.2 |
71 |
|
November 2020 |
11914 |
3685.8 |
784 |
|
December 2020 |
17109 |
8172.0 |
1607 |
|
January 2021 |
12538 |
2056.8 |
818 |
|
February 2021 |
10085 |
867.6 |
429 |
|
March 2021 |
12767 |
3533 |
845 |
|
April 2021 |
12584 |
4119 |
1067 |
|
May 2021 |
9977 |
1778.2 |
517 |
|
June 2021 |
8918 |
1145.8 |
182 |
|
July 2021 |
8452 |
473.8 |
67 |
|
August 2021 |
8379 |
560.8 |
178 |
|
September 2021 |
11756 |
4308.6 |
932 |
|
October 2021 |
15653 |
7161.2 |
1721 |
|
November 2021 |
13808 |
5579.8 |
1736 |
|
December 2021 |
11705 |
2768 |
1023 |
|
January 2022 |
11392 |
910.8 |
915 |
|
February 2022 |
13094 |
3876.6 |
1612 |
|
March 2022 |
11250 |
2016 |
558 |
|
April 2022 |
8479 |
14 |
192 |
|
May 2022 |
8387 |
188.2 |
90 |
|
June 2022 |
7744 |
-28.2* |
45 |
Note: Author calculation based on data from RZS .
* Negative value means that fewer deaths occured in given month compared with baseline period
From March 2020 until June 2022, 16 136 Covid-19 deaths and 2 029 403 confirmed cases were registered in Serbia. Since the first case of Covid-19 was reported in Serbia, all months registered Covid-19 mortality. The highest numbers of Covid-19 deaths were registered in October and November 2021, while the lowest Covid-19 deaths were in March, June and September 2020. Analysis of excess deaths shows slightly different monthly pattern, respectively highest excess death was recorded in December 2020 and October and November 2021 (Table 1). Also, data for March and May 2020, as well as for June 2022 didn t show excess death.

Figure 2. Estimated excess mortality rate in Serbia, from January 2015 to June 2022
Observing excess death during the pandemic period only, can not provide complete perception of excess mortality. In order to achieve better understanding, excess mortality rate was calculated from the 2015. Figure 2 shows estimated excess mortality rate on monthly level, while with red line was marked period before and after Covid-19 pandemic has started. From January 2015 until the March 2020, excess mortality was observed in some months, but there were also months where excess deaths were not registered (Figure 2). In this period, 38 months were observed without excess deaths, and in months with excess deaths-almost in all months excess mortality rate was below 12%. Only outlier were December 2016 with excess mortality rate of 12.7% and January 2017, with excess mortality rate of 44.2%. Namely, in January 2017, observed number of death was 44% higher than expected, when the seasonal flu in the winter 2016/17 was spread all over Europe. Mortality is not uniform during the year and seasonal changes are well known with higher mortality rate during the winter (Arsenović, 2018; Healy, 2003; Marti-Soler et al., 2014). Seasonal pattern of mortality is related with different drivers, and one of them is flu (Iuliano et al. 2018; Portugal 2021). Winter season 2016/17 in Europe was characterized with influenza-associated mortality (Josipovič, 2021; Nielsen et al., 2018) and increase in excess deaths particularly among elderly (Rosano et al. ,2019).
Since the March 2020, excess mortality rate has significant increase, with highest values in December 2020 (91.4%), October (84.3) and November (67.8) 2021. High value of excess mortality rate were estimated also in November 2020 (44.8), April 2021 (48.7), September 2021 (57.9) and February 2022 (42.1). Excess mortality rate above 20% was also registered in July 2020, March, May and December 2021 and March 2022 (Figure 2).
Since the beginning of COVID-19 pandemic, all countries in Europe experienced higher excess mortality compared to the period before 2020, with apparent regional differences. Regardless to the fact that first wave of pandemic has most harvesting impact for population in countries located in Western and South Europe, study for 2020-21, conducted by Wang et al. (2022), shows that highest reported Covid-19 mortality rate and estimated excess mortality rate were observed in countries of Central and Eastern Europe.
According to Eurostat, between March 2020 and June 2022, the EU recorded four peaks of excess mortality4: April 2020 (25.2%), November 2020 (40%), April 2021 (20.9%) and November 2021 (26.5%). At the beginning, in March-April 2020 the highest peak of excess mortality was in Italy, Spain, then France, Belgium and Netherlands, and according to some authors (Kontis et al., 2020; Konstantinoudis et al., 2022) in England and Wales too. In Spain, during the first wave, MoMo estimated 44 583 excess deaths (Leon.Gomez et al., 2021). While for the same period, in Italy, Dorrucci et al. (2021) estimated 52 437 excess deaths. In Portugal, between March 16 and April 14 in 2020, observed mortality was 14% higher than expected, respectively excess of 1 255 all-cause deaths (Vieira et al., 2020). Analysis for Belgium, conducted by Bustos Sierra et al, (2020), indicated that during the first wave in 2020, 96% of the excess mortality were likely attributable to Covid-19. Results for England and Wales show that in the first half of 2020, apart from the official Covid-19 death, there were an additional 968 weekly deaths (Vandoros, 2020). Until the end of 2020, geographical prevalence was in Eastern Europe, with highest peaks in Poland, Bulgaria and Slovenia4. During this second wave, Serbia also recorded a high excess mortality rate witha peak in December 2020 (91.4%). Third peak EU reached in April 2021 (20.9%)4, the same month as in Serbia with a 48.7% excess mortality rate. In following summer period 2021 all countries in Europe, including Serbia, had decreasing trend in excess mortality, while the autumn period recorded new increase for EU in September (12.9%) and for Serbia in October (84.3%). This was fourth wave which as extended to the first months of 2022 when excess mortality weakened in most of EU countries4. In Serbia, fourth wave has peak in February 2022 (42.1%).
Excess mortality was also reported in studies focusing on the regional level, but with large intra-country divergency (Blangiardo et al. 2020; Konstatinoudis et al., 2022). In Italy and Greece northern regions were more affected with highest excess mortality compared to the other parts of country. In Spain, regions Madrid, Castile-la Mancha and Castile-Leon, in England regions Outer London and West Midlands and in Switzerland region Ticino were most affected (Konstantinoudis et al., 2022). Regional variations of case-fatality rates in Germany shows considerably higher risk in eastern federal states (Morwinsky et al., 2021). Regional analysis of Covid-19 deaths, in 2020, in Serbia confirmed highest fatality effects in south region of country, but also in area of large cities such as Belgrade, Kragujevac and Nis (Marinković, 2021b).
Study, like one conducted for Belgium population founded that monthly mortality during the Covid-19 was higher than the number of monthly deaths during the influenza pandemic in late 1970s. According to the same study, compared to the April 2020, higher number of deaths in Belgium was recorded in World War II and during the Spanish influenza (Sierra et al. 2020). As the Covid-19 is one of the greatest pandemic since the beginning of 20st century, various studies follow impact and patterns between Covid-19 and Spanish fly pandemic. First Covid-19 wave was quite equal with major wave of the 1918-19 influenza in context of similar magnitude and length (He et al., 2020). While estimation of mortality shows that Spanish fly had higher number of death relative to population size and caused more significant loss of remaining life expectancy due to the fact that 1918 pandemic were killed many of middle-aged population (Goldstein & Lee, 2020).
Conclusion
Seasonal variation in mortality followed by excess mortality are well recognized and established, following U or V shape mostly, with higher mortality during the colder period of the year. Simultaneously, excess mortality could be found during the both-cold and hot weather, forming seasonal patterns. Different socio-demographic (age, gender, marital status, education, occupation) and medical (seasonal flu, pre-existing chronic diseases etc) factors shape excess mortality too. In order to assess the Covid-19 impact on mortality, analysis in this paper was based on excess mortality. Relative to the Covid-19 death, excess mortality is more convenient measure of total impact of the pandemic, considering that excess mortality could captures Covid-19 deaths that are „covered“ or unestimated due to not correctly diagnoses, and other causes that can be attributed to the overall crisis.
Results in this paper shows that Covid-19 has an impact on excess mortality, and since the beginning of March 2020 monthly excess mortality rate has a higher value compared to the historical baseline period. Analysis in this paper does not observe other anomalies that could be related with excess mortality, which imply that not all excess deaths could be referred to Covid-19.
Nevertheless, severity of Covid-19 pandemic imply continously accurate measurement of death including excess mortality, for better understanding of variations in excess mortality, giving strong evidence for public health threaths.
Acknowledgement
This research has been contributed by the Ministry of Education, Science and Technological Development of the Republic of Serbia through the Project No. 451-03-68/2022-14/200125.
References
Arsenović, D. (2020). COVID-19 in Serbia: demographic reflection and response. Demographic Aspects of COVID-19 Pandemic and its Consequences, 30 November – 1 December, Vienna, Austria. https://www.oeaw.ac.at/vid/events/calendar/conferences/demographic-aspects-of-the-covid-19-pandemic-and-its-consequences
Arsenović, D. (2021). Demographic aspects of mortality during the Covid-19 pandemic in Serbia. The 5th Serbian congress of geographers: Innovative approach and perspectives of the applied geography, 9-11 September, Novi Sad, Serbia. ISBN 978-86-7031-588-4.
Arsenović, D. (2018). Seasonality in human mortality: results for the City of Novi Sad (Serbia). Stanovništvo 56(1), 27-42. doi.org/10.2298/STNV1801027A
Balbo, N., Kashnitsky, I., Melegaro, A., Meslé, F., Mills, M. C., de Valk, H., & Vono de Vilhena, D. (2020). Demography and the coronavirus pandemic. Population & policy compact: policy brief, 25.
Beaney, T., Clarke, J. M., Jain, V., Golestaneh, A. K., Lyons, G., Salman, D. & Majeed, A. (2020). Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? Journal of the Royal Society of Medicine 113(9), 329–334. doi.org/10.1177/0141076820956802
Blangiardo, M., Cameletti, M., Pirani, M., Corsetti, G., Battaglini, M., & Baio, G. (2020). Estimating weekly excess mortality at sub-national level in Italy during the COVID-19 pandemic. PloS one, 15(10), e0240286. doi:https://doi.org/10.1371/journal.pone.0240286
Boukhris, M., Hillani, A., Moroni, F., Annabi, M. S., Addad, F., Ribeiro, M. H., Mansour, S., Zhao, X., Ybarra, L.F., Abbate, A., Vilca, M.L., & Azzalini, L. (2020). Cardiovascular implications of the COVID-19 pandemic: a global perspective. Canadian Journal of Cardiology 36(7), 1068-1080. https://doi.org/10. 1016/j.cjca.2020.05.018 PMID: 32425328.
Bustos Sierra, N., Bossuyt, N., Braeye, T., Leroy, M., Moyersoen, I., Peeters, I., Scohy, A., Van der Heyden, J., Van Oyen, H., & Renard, F. (2020). All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. Archives of Public Health 78(117), 1-8. doi.org/10.1186/s13690-020-00496-x
Del Pinto, R., Ferri, C., Mammarella, L., Abballe, S., Dell’Anna, S., Cicogna, S., Grassi, D., Sacco, S., & Desideri, G. (2020). Increased cardiovascular death rates in a COVID–19 low prevalence area. The Journal of Clinical Hypertension, 22(10), 1932-1935. https://doi.org/10. 1111/jch.14013 PMID: 32815667
Driggin, E., Madhavan, M. V., Bikdeli, B., Chuich, T., Laracy, J., Biondi-Zoccai, G., Brown, S.T., Der Nigoghossian C., Zidar, A.D., Haythe, J., Brodie, D., Beckman, A.S., Kirtane, A.J., Stone, W.G., Krumholz, M.H., & Parikh, S. A. (2020). Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. Journal of the American College of cardiology 75(18), 2352-2371. https://doi.org/10.1016/j.jacc.2020.03.031 PMID: 32201335
Dong, E., Du, H., & Gardner, L. (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet infectious diseases 20(5), 533-534. https://doi.org/10.1016/S1473-3099(20)30120-1
Dorrucci, M., Minelli, G., Boros, S., Manno, V., Prati, S., Battaglini, M., Corsetti, G., Andrianou, X., Riccardo, F., Fabiani, M., Vescio, F.M., Spuri, M., Mateo-Urdiales, A., Del Manso, M., Onder, G., Pezzotti, P., & Bella, A. (2021). Excess mortality in Italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Frontiers in public health 927(9), 669209. doi: 10.3389/fpubh.2021.669209.
Dowd, J. B., Andriano, L., Brazel, D. M., Rotondi, V., Block, P., Ding, X., Liu, Y., & Mills, M. C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences, 117(18), 9696-9698, 202004911. doi: 10.1073/pnas.2004911117
Islam, N., Shkolnikov, VM., Acosta, RJ., Klimkin, I., Kawachi, I., Irizarry, RA., Alicandro, G., Khunti, K., Yates, T., Jdanov, DA., White, M., Lewington, S. & Lacey, B. (2021). Excess deaths associated with covid-19 pandemic in 2020: age and seks disaggregated time series analysis in 29 high income countries. British Medical Journal 373, n1137. doi: https://doi.org/10.136/bmj.n1137, PMID: 34011491.
Josipovič, D. (2021). COVID-19 and excess mortality: Was it possible to lower number of deaths in Slovenia?. Stanovništvo 59(1), 17-30. doi.org/10.2298/STNV2101017J
Iuliano, A. D., Roguski, K. M., Chang, H. H., Muscatello, D. J., Palekar, R., Tempia, S., … & Mustaquim, D. (2018). Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. The Lancet 391(10127), 1285-1300. doi: 10.1016/S0140-6736(17)33293-2.
León-Gómez, I., , C., , C., L., , L., , A. & Larrauri, A. (2021). The Impact of COVID-19 on Mortality in Spain: Monitoring Excess Mortality (MoMo) and the Surveillance of Confirmed COVID-19 Deaths. Viruses 13(12), 2423. doi: 10.3390/v13122423.
Konstantinoudis, G., Cameletti, M., Gómez-Rubio, V., León Gómez, I., Pirani, M., Baio, G., Larrauri, A., Riou, J., Egger, M., Vineis, P. & Blangiardo, M. (2022). Regional excess mortality during the 2020 COVID-19 pandemic in five European countries. Nature Communications 13, 482. doi.org/10.1038/s41467-022-28157-3.
Kontis, V., Bennett, J. E., Rashid, T., Parks, R. M., Pearson-Stuttard, J., Guillot, M., Asaria, P., Zhou, B., Battaglini, M., Corsetti, G., McKee, M., Di Cesare, M., Mathers, D.C., & Ezzati, M. (2020). Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nature medicine, 26(12), 1919-1928. doi.org/10.1038/s41591-020-1112-0
Kustudic, M., Niu, B., & Liu, Q. (2021). Agent-based analysis of contagion events according to sourcing locations. Scientific Reports 11(1), 16032. doi.org/10.1038/s41598-021-95336-5
Gill, J. R., & DeJoseph, M. E. (2020). The importance of proper death certification during the COVID-19 pandemic. Jama 324(1), 06032. https://doi.org/10.1001/jama.2020.9536 PMID: 32520302
Goldstein, J. R., & Lee, R. D. (2020). Demographic perspectives on the mortality of COVID-19 and other epidemics. Proceedings of the National Academy of Sciences 117(36), 22035-22041. https://doi.org/10.1073/pnas.2006392117
Healy, J.D. (2003). Excess winter mortality in Europe: a cross-country analysis identifying key risk factors. Journal of Epidemiology and Community Health 57(10), 784-789. doi.org/10.1136/jech.57.10.784
He, D., Zhao, S., Li, Y., Cao, P., Gao, D., Lou, Y. & Yang, L. (2020). Comparing Covid-19 and the influenza pandemics in the United Kingdom. International Journal of Infectious Diseases 98, 67-70. https://doi.org/10.1016/j.ijid.2020.06.075
Hulikova Tesarkova, K. (2020). Demographic aspects of the Covid-19 pandemic in Italy, Spain, Germany and South Korea. Geografie 125(2), 139-170. doi.org/10.37040/geografie2020125020139
Marti-Soler, H., Gonseth, S., Gubelmann, C., Stringhini, S., Bovet, P., Chen, P.C., Wojtyniak, B., Paccaud, F., Tsai, D.H., Zdrojewski, T. & Marques-Vidal, P. (2014). Seasonal Variation of Overall and Cardiovascular Mortality: A Study in 19 Countries from Different Geographic Locations. PLOSone 9(11), doi:10.1371/ journal.pone.0113500
Marinković, I. & Galjak, M. (2021a). Prekomerna smrtnost u godini pandemije 2020. U Evropi i Srbiji. Stanovništvo 59(1), 61-73. doi.org/10.2298/STNV2101061M
Marinković, I. (2021b). Regionalna analiza smrtnosti od Covid-19 u Srbiji 2020. Demografija 18, 39-56. doi: 10.5937/demografija2118001M
Michalek, A. (2022). Spatially differentiated impacts of Covid-19 on selected indicators of mortality in Slovakia in 2020. Geographica Pannonica 26(2), 112-127. doi: 10.5937/gp26-37578
Michelozzi, P., De’Donato, F., Scortichini, M., Pezzotti, P., Stafoggia, M., De Sario, M., Costa, G., Noccioli, F., Riccardo, F., Bella, A., Demaria, M., Rossi, P., Brusaferro, S., Rezza, G. & Davoli, M. (2020). Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health, 20,1238. doi.org/10.1186/s12889-020-09335-8
Mogi, R., & Spijker, J. (2022). The influence of social and economic ties to the spread of COVID-19 in Europe. Journal of Population Research 39(4), 495-511. doi.org/10.1007/s12546-021-09257-1
Morwinsky, S., Nitsche, N. & Acosta E. (2021). COVID-19 fatality in Germany: Demographic determinants of variation in case-fatality rates across and within German federal states during the first and second waves. Demographic research 45, 1355-1372. doi: 10.4054/DemRes.2021.45.45
Nielsen, J., Krause ,T.G. & Molbak K. (2018). Influenza-associated mortality determined from all-cause mortality, Denmark, 2010/11-2016/17: The FluMOMO model. Influenza and other respirtory viruses 12(5), 591-604. https://doi.org/10.1111%2Firv.12564
Portugal, L. (2021). Mortality and Excess Mortality: Improving FluMOMO. Journal of Environmental and Public Health 5582589, 1-8. doi.org/10.1155/2021/5582589
Rosano, A., Bella, A., Gesualdo, F., Acampora, A., Pezzotti, P., Marchetti, S., Ricciardi, W. & Rizzo C. (2019). Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14-2016/17 seasons). International Journal of infectious Diseases 88, 127-134. doi.org/10.1016/j.ijid.2019.08.003
RZS (2022). Statistika stanovništva [Population Statistics Report]. No. 206. 25.07.2022. ISSN 0353-9555.
Stokes, C.A., Lundberg, J.D., Elo, T.I., Hempstead, K., Bor, J. & Preston, H.S. (2021). Covid-19 excess mortality in the United States: A country-level analysis. PLoS Medicine 18(5), e1003571. https://doi.org/10.1371/journal.pmed.1003571
Sher, L. (2020). The impact of the COVID-19 pandemic on suicide rates. QJM: An International Journal of Medicine, 113(10), 707-712. https://doi.org/10.1093/qjmed/hcaa202 PMID: 32539153
SORS (2015). Demographic Yearbook in the Republic of Serbia 2014. Belgrade: Serbia. ISSN 0084-4357.
Vandoros, S. (2020). Excess mortality during the Covid-19 pandemic: Early evidence from England and Wales. Social Science & Medicine 258, 113101. https://doi.org/10.1016/j.socscimed.2020.113101
Vieira, A., Ricoca Peixoto, V., Aguiar, P. & Abrantes, A. (2020). Rapid Estimation of Excess Mortality during the COVID-19 Pandemic in Portugal-Beyond Reported Deaths. Journal of Epidemiology and Global Health 10(3), 209-313. https://doi.org/10.2991/jegh.k.200628.001
Wang, H., Paulson, K. R., Pease, S. A., Watson, S., Comfort, H., Zheng, P., … & Murray, C. J. (2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet 399(10334), 1513-1536. https://doi.org/10.1016/S0140-6736(21)02796-3
1 Source: WHO, July 20 2022 (www.covid19.who.int)
In this paper, the historical baseline consists of the average number of deaths that occured in each month in the five year period before observed year. Excess mortality for the 2020, 2021 and first half of 2022 was calculated using historical baseline from previous years in a period which was not affected by the Covid-19, considering the number of deaths that occurred in each month during the period 2015-2019.
Results and discussion
Serbia reported the first case of Covid-19 on the 6th March 2020. Nine days later (March 15th), a state of emergency was declared in the country and in order to reduce transmission, the whole population was lockdown. All public sectors were redirected to telecommuting, while other places of services and for public gathering were closed. Regardless of all country-wide measures during March 2020, transmission of Covid-19 was very fast and intense. Fast transmission in this period could be related to the fact that about 300,000 of Serbian residents arrived from abroad (Arsenović, 2020). After two months, on May 7th 2020, the government ended the state of emergency, with recommendation and not very restrictive social distancing. Since second half of June 2020, large-scale testing was conducted and the number of new confirmed cases and number of deaths due to Covid-19 has started to increase (Arsenović, 2020). During the second half of 2020 and the whole 2021 government applied different restrictions regarding the reduced or limited working time in public administration and services (e.g. restaurants, bars and markets), but without lockdown. Since the beginning of 2022 these restrictions have been withdrawn.
With exception in February, the average number of monthly deaths during the Covid-19 pandemic years 2020-21 was higher in all other months compared to the average number of monthly deaths in two preceding years 2018-19 (Figure 1). Divergence in average number of monthly deaths has ranged from 665 (in August) to 5 665 (in December) when it was recorded the highest number of deaths and excess deaths too.
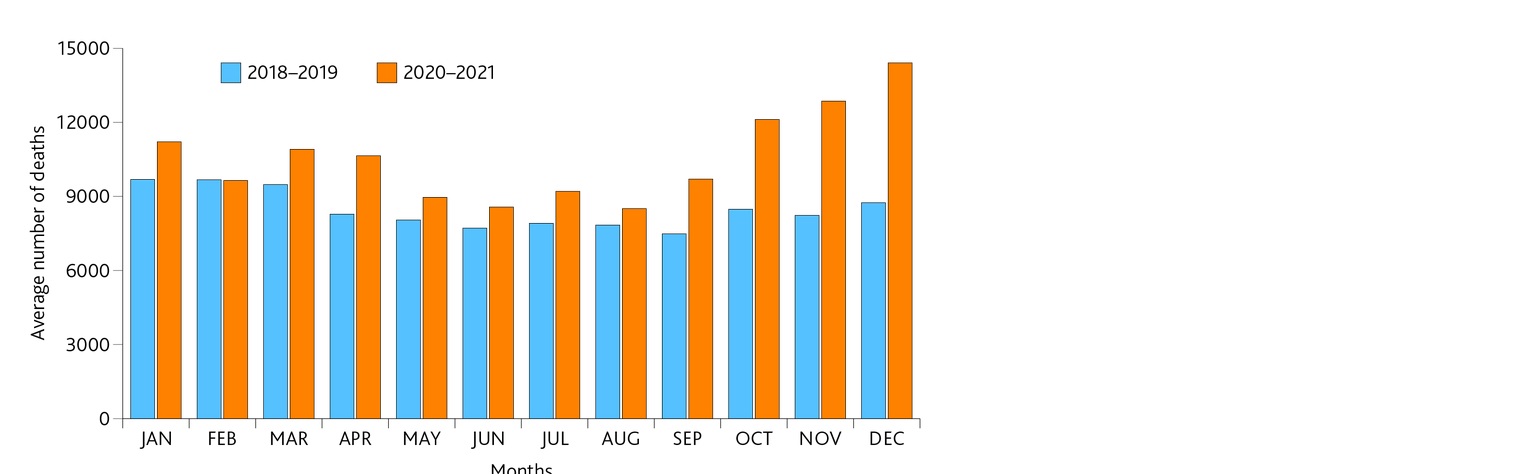
Figure 1. Average number of death per month in 2018-19 and 2020-21
Note: Author calculation based on data from RZS and Covid-19 database
Table 1. Estimated excess mortality and number of confirmed deaths from Covid-19, March 2020-June 2022
|
Month |
Observed number of deaths |
Excess deaths |
Number of confirmed deaths from Covid-19 |
|
March 2020 |
9050 |
-184.0* |
23 |
|
April 2020 |
8710 |
245.0 |
154 |
|
May 2020 |
7943 |
-255.8* |
64 |
|
June 2020 |
8222 |
449.8 |
34 |
|
July 2020 |
9959 |
1980.8 |
296 |
|
August 2020 |
8626 |
807.8 |
140 |
|
September 2020 |
7646 |
198.6 |
36 |
|
October 2020 |
8580 |
88.2 |
71 |
|
November 2020 |
11914 |
3685.8 |
784 |
|
December 2020 |
17109 |
8172.0 |
1607 |
|
January 2021 |
12538 |
2056.8 |
818 |
|
February 2021 |
10085 |
867.6 |
429 |
|
March 2021 |
12767 |
3533 |
845 |
|
April 2021 |
12584 |
4119 |
1067 |
|
May 2021 |
9977 |
1778.2 |
517 |
|
June 2021 |
8918 |
1145.8 |
182 |
|
July 2021 |
8452 |
473.8 |
67 |
|
August 2021 |
8379 |
560.8 |
178 |
|
September 2021 |
11756 |
4308.6 |
932 |
|
October 2021 |
15653 |
7161.2 |
1721 |
|
November 2021 |
13808 |
5579.8 |
1736 |
|
December 2021 |
11705 |
2768 |
1023 |
|
January 2022 |
11392 |
910.8 |
915 |
|
February 2022 |
13094 |
3876.6 |
1612 |
|
March 2022 |
11250 |
2016 |
558 |
|
April 2022 |
8479 |
14 |
192 |
|
May 2022 |
8387 |
188.2 |
90 |
|
June 2022 |
7744 |
-28.2* |
45 |
From March 2020 until June 2022, 16 136 Covid-19 deaths and 2 029 403 confirmed cases were registered in Serbia. Since the first case of Covid-19 was reported in Serbia, all months registered Covid-19 mortality. The highest numbers of Covid-19 deaths were registered in October and November 2021, while the lowest Covid-19 deaths were in March, June and September 2020. Analysis of excess deaths shows slightly different monthly pattern, respectively highest excess death was recorded in December 2020 and October and November 2021 (Table 1). Also, data for March and May 2020, as well as for June 2022 didn t show excess death.
Figure 2. Estimated excess mortality rate in Serbia, from January 2015 to June 2022
Observing excess death during the pandemic period only, can not provide complete perception of excess mortality. In order to achieve better understanding, excess mortality rate was calculated from the 2015. Figure 2 shows estimated excess mortality rate on monthly level, while with red line was marked period before and after Covid-19 pandemic has started. From January 2015 until the March 2020, excess mortality was observed in some months, but there were also months where excess deaths were not registered (Figure 2). In this period, 38 months were observed without excess deaths, and in months with excess deaths-almost in all months excess mortality rate was below 12%. Only outlier were December 2016 with excess mortality rate of 12.7% and January 2017, with excess mortality rate of 44.2%. Namely, in January 2017, observed number of death was 44% higher than expected, when the seasonal flu in the winter 2016/17 was spread all over Europe. Mortality is not uniform during the year and seasonal changes are well known with higher mortality rate during the winter (Arsenović, 2018; Healy, 2003; Marti-Soler et al., 2014). Seasonal pattern of mortality is related with different drivers, and one of them is flu (Iuliano et al. 2018; Portugal 2021). Winter season 2016/17 in Europe was characterized with influenza-associated mortality (Josipovič, 2021; Nielsen et al., 2018) and increase in excess deaths particularly among elderly (Rosano et al. ,2019).
Since the March 2020, excess mortality rate has significant increase, with highest values in December 2020 (91.4%), October (84.3) and November (67.8) 2021. High value of excess mortality rate were estimated also in November 2020 (44.8), April 2021 (48.7), September 2021 (57.9) and February 2022 (42.1). Excess mortality rate above 20% was also registered in July 2020, March, May and December 2021 and March 2022 (Figure 2).
Since the beginning of COVID-19 pandemic, all countries in Europe experienced higher excess mortality compared to the period before 2020, with apparent regional differences. Regardless to the fact that first wave of pandemic has most harvesting impact for population in countries located in Western and South Europe, study for 2020-21, conducted by Wang et al. (2022), shows that highest reported Covid-19 mortality rate and estimated excess mortality rate were observed in countries of Central and Eastern Europe.
According to Eurostat, between March 2020 and June 2022, the EU recorded four peaks of excess mortality4: April 2020 (25.2%), November 2020 (40%), April 2021 (20.9%) and November 2021 (26.5%). At the beginning, in March-April 2020 the highest peak of excess mortality was in Italy, Spain, then France, Belgium and Netherlands, and according to some authors (Kontis et al., 2020; Konstantinoudis et al., 2022) in England and Wales too. In Spain, during the first wave, MoMo estimated 44 583 excess deaths (Leon.Gomez et al., 2021). While for the same period, in Italy, Dorrucci et al. (2021) estimated 52 437 excess deaths. In Portugal, between March 16 and April 14 in 2020, observed mortality was 14% higher than expected, respectively excess of 1 255 all-cause deaths (Vieira et al., 2020). Analysis for Belgium, conducted by Bustos Sierra et al, (2020), indicated that during the first wave in 2020, 96% of the excess mortality were likely attributable to Covid-19. Results for England and Wales show that in the first half of 2020, apart from the official Covid-19 death, there were an additional 968 weekly deaths (Vandoros, 2020). Until the end of 2020, geographical prevalence was in Eastern Europe, with highest peaks in Poland, Bulgaria and Slovenia4. During this second wave, Serbia also recorded a high excess mortality rate witha peak in December 2020 (91.4%). Third peak EU reached in April 2021 (20.9%)4, the same month as in Serbia with a 48.7% excess mortality rate. In following summer period 2021 all countries in Europe, including Serbia, had decreasing trend in excess mortality, while the autumn period recorded new increase for EU in September (12.9%) and for Serbia in October (84.3%). This was fourth wave which as extended to the first months of 2022 when excess mortality weakened in most of EU countries4. In Serbia, fourth wave has peak in February 2022 (42.1%).
Excess mortality was also reported in studies focusing on the regional level, but with large intra-country divergency (Blangiardo et al. 2020; Konstatinoudis et al., 2022). In Italy and Greece northern regions were more affected with highest excess mortality compared to the other parts of country. In Spain, regions Madrid, Castile-la Mancha and Castile-Leon, in England regions Outer London and West Midlands and in Switzerland region Ticino were most affected (Konstantinoudis et al., 2022). Regional variations of case-fatality rates in Germany shows considerably higher risk in eastern federal states (Morwinsky et al., 2021). Regional analysis of Covid-19 deaths, in 2020, in Serbia confirmed highest fatality effects in south region of country, but also in area of large cities such as Belgrade, Kragujevac and Nis (Marinković, 2021b).
Study, like one conducted for Belgium population founded that monthly mortality during the Covid-19 was higher than the number of monthly deaths during the influenza pandemic in late 1970s. According to the same study, compared to the April 2020, higher number of deaths in Belgium was recorded in World War II and during the Spanish influenza (Sierra et al. 2020). As the Covid-19 is one of the greatest pandemic since the beginning of 20st century, various studies follow impact and patterns between Covid-19 and Spanish fly pandemic. First Covid-19 wave was quite equal with major wave of the 1918-19 influenza in context of similar magnitude and length (He et al., 2020). While estimation of mortality shows that Spanish fly had higher number of death relative to population size and caused more significant loss of remaining life expectancy due to the fact that 1918 pandemic were killed many of middle-aged population (Goldstein & Lee, 2020).
Conclusion
Seasonal variation in mortality followed by excess mortality are well recognized and established, following U or V shape mostly, with higher mortality during the colder period of the year. Simultaneously, excess mortality could be found during the both-cold and hot weather, forming seasonal patterns. Different socio-demographic (age, gender, marital status, education, occupation) and medical (seasonal flu, pre-existing chronic diseases etc) factors shape excess mortality too. In order to assess the Covid-19 impact on mortality, analysis in this paper was based on excess mortality. Relative to the Covid-19 death, excess mortality is more convenient measure of total impact of the pandemic, considering that excess mortality could captures Covid-19 deaths that are „covered“ or unestimated due to not correctly diagnoses, and other causes that can be attributed to the overall crisis.
Results in this paper shows that Covid-19 has an impact on excess mortality, and since the beginning of March 2020 monthly excess mortality rate has a higher value compared to the historical baseline period. Analysis in this paper does not observe other anomalies that could be related with excess mortality, which imply that not all excess deaths could be referred to Covid-19.
Nevertheless, severity of Covid-19 pandemic imply continously accurate measurement of death including excess mortality, for better understanding of variations in excess mortality, giving strong evidence for public health threaths.
Acknowledgement
This research has been contributed by the Ministry of Education, Science and Technological Development of the Republic of Serbia through the Project No. 451-03-68/2022-14/200125.
References
Arsenović, D. (2020). COVID-19 in Serbia: demographic reflection and response. Demographic Aspects of COVID-19 Pandemic and its Consequences, 30 November – 1 December, Vienna, Austria. https://www.oeaw.ac.at/vid/events/calendar/conferences/demographic-aspects-of-the-covid-19-pandemic-and-its-consequences
Arsenović, D. (2021). Demographic aspects of mortality during the Covid-19 pandemic in Serbia. The 5th Serbian congress of geographers: Innovative approach and perspectives of the applied geography, 9-11 September, Novi Sad, Serbia. ISBN 978-86-7031-588-4.
Arsenović, D. (2018). Seasonality in human mortality: results for the City of Novi Sad (Serbia). Stanovništvo 56(1), 27-42. doi.org/10.2298/STNV1801027A
Balbo, N., Kashnitsky, I., Melegaro, A., Meslé, F., Mills, M. C., de Valk, H., & Vono de Vilhena, D. (2020). Demography and the coronavirus pandemic. Population & policy compact: policy brief, 25.
Beaney, T., Clarke, J. M., Jain, V., Golestaneh, A. K., Lyons, G., Salman, D. & Majeed, A. (2020). Excess mortality: the gold standard in measuring the impact of COVID-19 worldwide? Journal of the Royal Society of Medicine 113(9), 329–334. doi.org/10.1177/0141076820956802
Blangiardo, M., Cameletti, M., Pirani, M., Corsetti, G., Battaglini, M., & Baio, G. (2020). Estimating weekly excess mortality at sub-national level in Italy during the COVID-19 pandemic. PloS one, 15(10), e0240286. doi:https://doi.org/10.1371/journal.pone.0240286
Boukhris, M., Hillani, A., Moroni, F., Annabi, M. S., Addad, F., Ribeiro, M. H., Mansour, S., Zhao, X., Ybarra, L.F., Abbate, A., Vilca, M.L., & Azzalini, L. (2020). Cardiovascular implications of the COVID-19 pandemic: a global perspective. Canadian Journal of Cardiology 36(7), 1068-1080. https://doi.org/10. 1016/j.cjca.2020.05.018 PMID: 32425328.
Bustos Sierra, N., Bossuyt, N., Braeye, T., Leroy, M., Moyersoen, I., Peeters, I., Scohy, A., Van der Heyden, J., Van Oyen, H., & Renard, F. (2020). All-cause mortality supports the COVID-19 mortality in Belgium and comparison with major fatal events of the last century. Archives of Public Health 78(117), 1-8. doi.org/10.1186/s13690-020-00496-x
Del Pinto, R., Ferri, C., Mammarella, L., Abballe, S., Dell’Anna, S., Cicogna, S., Grassi, D., Sacco, S., & Desideri, G. (2020). Increased cardiovascular death rates in a COVID–19 low prevalence area. The Journal of Clinical Hypertension, 22(10), 1932-1935. https://doi.org/10. 1111/jch.14013 PMID: 32815667
Driggin, E., Madhavan, M. V., Bikdeli, B., Chuich, T., Laracy, J., Biondi-Zoccai, G., Brown, S.T., Der Nigoghossian C., Zidar, A.D., Haythe, J., Brodie, D., Beckman, A.S., Kirtane, A.J., Stone, W.G., Krumholz, M.H., & Parikh, S. A. (2020). Cardiovascular considerations for patients, health care workers, and health systems during the COVID-19 pandemic. Journal of the American College of cardiology 75(18), 2352-2371. https://doi.org/10.1016/j.jacc.2020.03.031 PMID: 32201335
Dong, E., Du, H., & Gardner, L. (2020). An interactive web-based dashboard to track COVID-19 in real time. The Lancet infectious diseases 20(5), 533-534. https://doi.org/10.1016/S1473-3099(20)30120-1
Dorrucci, M., Minelli, G., Boros, S., Manno, V., Prati, S., Battaglini, M., Corsetti, G., Andrianou, X., Riccardo, F., Fabiani, M., Vescio, F.M., Spuri, M., Mateo-Urdiales, A., Del Manso, M., Onder, G., Pezzotti, P., & Bella, A. (2021). Excess mortality in Italy during the COVID-19 pandemic: assessing the differences between the first and the second wave, year 2020. Frontiers in public health 927(9), 669209. doi: 10.3389/fpubh.2021.669209.
Dowd, J. B., Andriano, L., Brazel, D. M., Rotondi, V., Block, P., Ding, X., Liu, Y., & Mills, M. C. (2020). Demographic science aids in understanding the spread and fatality rates of COVID-19. Proceedings of the National Academy of Sciences, 117(18), 9696-9698, 202004911. doi: 10.1073/pnas.2004911117
Islam, N., Shkolnikov, VM., Acosta, RJ., Klimkin, I., Kawachi, I., Irizarry, RA., Alicandro, G., Khunti, K., Yates, T., Jdanov, DA., White, M., Lewington, S. & Lacey, B. (2021). Excess deaths associated with covid-19 pandemic in 2020: age and seks disaggregated time series analysis in 29 high income countries. British Medical Journal 373, n1137. doi: https://doi.org/10.136/bmj.n1137, PMID: 34011491.
Josipovič, D. (2021). COVID-19 and excess mortality: Was it possible to lower number of deaths in Slovenia?. Stanovništvo 59(1), 17-30. doi.org/10.2298/STNV2101017J
Iuliano, A. D., Roguski, K. M., Chang, H. H., Muscatello, D. J., Palekar, R., Tempia, S., … & Mustaquim, D. (2018). Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. The Lancet 391(10127), 1285-1300. doi: 10.1016/S0140-6736(17)33293-2.
León-Gómez, I., , C., , C., L., , L., , A. & Larrauri, A. (2021). The Impact of COVID-19 on Mortality in Spain: Monitoring Excess Mortality (MoMo) and the Surveillance of Confirmed COVID-19 Deaths. Viruses 13(12), 2423. doi: 10.3390/v13122423.
Konstantinoudis, G., Cameletti, M., Gómez-Rubio, V., León Gómez, I., Pirani, M., Baio, G., Larrauri, A., Riou, J., Egger, M., Vineis, P. & Blangiardo, M. (2022). Regional excess mortality during the 2020 COVID-19 pandemic in five European countries. Nature Communications 13, 482. doi.org/10.1038/s41467-022-28157-3.
Kontis, V., Bennett, J. E., Rashid, T., Parks, R. M., Pearson-Stuttard, J., Guillot, M., Asaria, P., Zhou, B., Battaglini, M., Corsetti, G., McKee, M., Di Cesare, M., Mathers, D.C., & Ezzati, M. (2020). Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nature medicine, 26(12), 1919-1928. doi.org/10.1038/s41591-020-1112-0
Kustudic, M., Niu, B., & Liu, Q. (2021). Agent-based analysis of contagion events according to sourcing locations. Scientific Reports 11(1), 16032. doi.org/10.1038/s41598-021-95336-5
Gill, J. R., & DeJoseph, M. E. (2020). The importance of proper death certification during the COVID-19 pandemic. Jama 324(1), 06032. https://doi.org/10.1001/jama.2020.9536 PMID: 32520302
Goldstein, J. R., & Lee, R. D. (2020). Demographic perspectives on the mortality of COVID-19 and other epidemics. Proceedings of the National Academy of Sciences 117(36), 22035-22041. https://doi.org/10.1073/pnas.2006392117
Healy, J.D. (2003). Excess winter mortality in Europe: a cross-country analysis identifying key risk factors. Journal of Epidemiology and Community Health 57(10), 784-789. doi.org/10.1136/jech.57.10.784
He, D., Zhao, S., Li, Y., Cao, P., Gao, D., Lou, Y. & Yang, L. (2020). Comparing Covid-19 and the influenza pandemics in the United Kingdom. International Journal of Infectious Diseases 98, 67-70. https://doi.org/10.1016/j.ijid.2020.06.075
Hulikova Tesarkova, K. (2020). Demographic aspects of the Covid-19 pandemic in Italy, Spain, Germany and South Korea. Geografie 125(2), 139-170. doi.org/10.37040/geografie2020125020139
Marti-Soler, H., Gonseth, S., Gubelmann, C., Stringhini, S., Bovet, P., Chen, P.C., Wojtyniak, B., Paccaud, F., Tsai, D.H., Zdrojewski, T. & Marques-Vidal, P. (2014). Seasonal Variation of Overall and Cardiovascular Mortality: A Study in 19 Countries from Different Geographic Locations. PLOSone 9(11), doi:10.1371/ journal.pone.0113500
Marinković, I. & Galjak, M. (2021a). Prekomerna smrtnost u godini pandemije 2020. U Evropi i Srbiji. Stanovništvo 59(1), 61-73. doi.org/10.2298/STNV2101061M
Marinković, I. (2021b). Regionalna analiza smrtnosti od Covid-19 u Srbiji 2020. Demografija 18, 39-56. doi: 10.5937/demografija2118001M
Michalek, A. (2022). Spatially differentiated impacts of Covid-19 on selected indicators of mortality in Slovakia in 2020. Geographica Pannonica 26(2), 112-127. doi: 10.5937/gp26-37578
Michelozzi, P., De’Donato, F., Scortichini, M., Pezzotti, P., Stafoggia, M., De Sario, M., Costa, G., Noccioli, F., Riccardo, F., Bella, A., Demaria, M., Rossi, P., Brusaferro, S., Rezza, G. & Davoli, M. (2020). Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health, 20,1238. doi.org/10.1186/s12889-020-09335-8
Mogi, R., & Spijker, J. (2022). The influence of social and economic ties to the spread of COVID-19 in Europe. Journal of Population Research 39(4), 495-511. doi.org/10.1007/s12546-021-09257-1
Morwinsky, S., Nitsche, N. & Acosta E. (2021). COVID-19 fatality in Germany: Demographic determinants of variation in case-fatality rates across and within German federal states during the first and second waves. Demographic research 45, 1355-1372. doi: 10.4054/DemRes.2021.45.45
Nielsen, J., Krause ,T.G. & Molbak K. (2018). Influenza-associated mortality determined from all-cause mortality, Denmark, 2010/11-2016/17: The FluMOMO model. Influenza and other respirtory viruses 12(5), 591-604. https://doi.org/10.1111%2Firv.12564
Portugal, L. (2021). Mortality and Excess Mortality: Improving FluMOMO. Journal of Environmental and Public Health 5582589, 1-8. doi.org/10.1155/2021/5582589
Rosano, A., Bella, A., Gesualdo, F., Acampora, A., Pezzotti, P., Marchetti, S., Ricciardi, W. & Rizzo C. (2019). Investigating the impact of influenza on excess mortality in all ages in Italy during recent seasons (2013/14-2016/17 seasons). International Journal of infectious Diseases 88, 127-134. doi.org/10.1016/j.ijid.2019.08.003
RZS (2022). Statistika stanovništva [Population Statistics Report]. No. 206. 25.07.2022. ISSN 0353-9555.
Stokes, C.A., Lundberg, J.D., Elo, T.I., Hempstead, K., Bor, J. & Preston, H.S. (2021). Covid-19 excess mortality in the United States: A country-level analysis. PLoS Medicine 18(5), e1003571. https://doi.org/10.1371/journal.pmed.1003571
Sher, L. (2020). The impact of the COVID-19 pandemic on suicide rates. QJM: An International Journal of Medicine, 113(10), 707-712. https://doi.org/10.1093/qjmed/hcaa202 PMID: 32539153
SORS (2015). Demographic Yearbook in the Republic of Serbia 2014. Belgrade: Serbia. ISSN 0084-4357.
Vandoros, S. (2020). Excess mortality during the Covid-19 pandemic: Early evidence from England and Wales. Social Science & Medicine 258, 113101. https://doi.org/10.1016/j.socscimed.2020.113101
Vieira, A., Ricoca Peixoto, V., Aguiar, P. & Abrantes, A. (2020). Rapid Estimation of Excess Mortality during the COVID-19 Pandemic in Portugal-Beyond Reported Deaths. Journal of Epidemiology and Global Health 10(3), 209-313. https://doi.org/10.2991/jegh.k.200628.001
Wang, H., Paulson, K. R., Pease, S. A., Watson, S., Comfort, H., Zheng, P., … & Murray, C. J. (2022). Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020–21. The Lancet 399(10334), 1513-1536. https://doi.org/10.1016/S0140-6736(21)02796-3
1 Source: WHO, July 20 2022 (www.covid19.who.int)